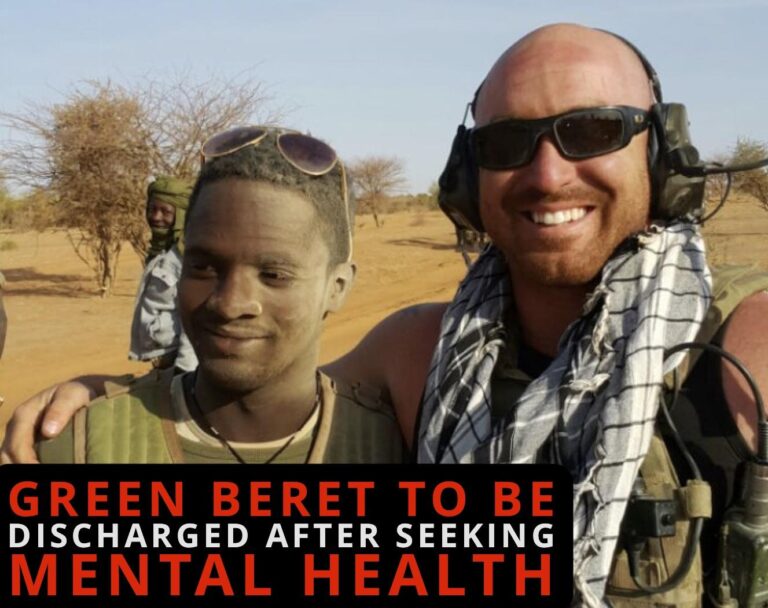
Veteran’s Mental Health Treatment Revealed in Las Vegas Cybertruck Explosion Case
Recent disclosures indicate that the former Green Beret involved in the widely reported Cybertruck explosion in Las Vegas was actively engaged in mental health care before the incident occurred. The veteran had been receiving treatment for symptoms related to anxiety and post-traumatic stress disorder (PTSD), conditions commonly experienced by military personnel after deployment. This new information adds complexity to the ongoing inquiry, emphasizing the mental health struggles many veterans endure during their reintegration into civilian society.
Investigators are currently focusing on several critical aspects, including:
- The accessibility and adequacy of mental health services available to veterans.
- Potential shortcomings in the monitoring and follow-up procedures for individuals undergoing PTSD treatment.
- The influence of social and familial support systems in mitigating crisis situations among former service members.
| Aspect | Current Status | Effect on Case |
|---|---|---|
| Mental Health Care | Active treatment ongoing | Provided some stability but incomplete support |
| Monitoring Procedures | Currently under evaluation | Identified potential gaps in oversight |
| Support Networks | Insufficient | Essential for crisis prevention |
Understanding the Mental Health Obstacles Veterans Face
The investigation into the Cybertruck explosion has brought renewed attention to the mental health difficulties that veterans frequently encounter. Despite their dedication and sacrifices, many veterans struggle with conditions such as PTSD, depression, and anxiety, which often require sustained psychological and medical intervention. According to the U.S. Department of Veterans Affairs, approximately 11-20% of veterans who served in Operations Iraqi Freedom and Enduring Freedom experience PTSD in a given year, highlighting the widespread nature of these challenges.
Several significant barriers hinder veterans from obtaining the care they need, including:
- Persistent stigma around mental health that discourages many from seeking assistance.
- Shortage of specialized treatment programs designed to address combat-related psychological trauma.
- Complex navigation of the Veterans Affairs (VA) healthcare system, which can delay timely access to services.
Below is a summary of prevalent mental health disorders among veterans, common obstacles to treatment, and suggested support strategies:
| Mental Health Condition | Typical Barriers | Recommended Interventions |
|---|---|---|
| Post-Traumatic Stress Disorder (PTSD) | Social stigma, fragmented care coordination | Complete therapy, peer-led support groups |
| Depression | Unrecognized symptoms, reluctance to seek help | Routine mental health screenings, accessible counseling services |
| Anxiety Disorders | Underdiagnosis, limited access to specialized care | Early detection, personalized medication and therapy plans |
Calls for Improved Mental Health Support Systems for Service Members
The circumstances surrounding the Green Beret’s involvement in the Cybertruck explosion highlight the pressing need for enhanced mental health care frameworks tailored to military personnel.Although the veteran was receiving treatment,this case reveals the difficulties service members face in accessing continuous,personalized,and stigma-free mental health support. Experts advocate for a more robust infrastructure that addresses these gaps effectively.
Key expert recommendations include:
- Introducing proactive mental health assessments at various stages throughout military service.
- Expanding confidential counseling options that accommodate the unique demands of active duty.
- Developing family-centered support initiatives to foster a comprehensive care environment.
- Increasing investment in research focused on PTSD and trauma-related disorders to improve treatment outcomes.
| Support Area | Current Condition | Suggested Enhancements |
|---|---|---|
| On-Duty Counseling | Limited availability | Increase access and extend service hours |
| Transition Support Post-Service | Inconsistent follow-up care | Implement mandatory post-discharge check-ins |
| Family Assistance Programs | Under-resourced | Create comprehensive education and support initiatives |
| Research Funding | Insufficient | Boost dedicated grants for mental health studies |
Advancing Mental Health Screening and Crisis Management for Veterans
Improving mental health outcomes for veterans requires integrating routine psychological evaluations into standard primary care appointments. This strategy helps normalize mental health discussions, reduces stigma, and facilitates early detection of symptoms before they escalate. Utilizing veteran-specific screening instruments such as the PTSD Checklist for DSM-5 (PCL-5) and the Patient Health Questionnaire (PHQ-9) enhances diagnostic accuracy. Additionally, expanding telehealth capabilities ensures veterans in rural or underserved areas can access timely mental health services without logistical barriers.
Effective crisis intervention demands a comprehensive approach, including the deployment of specialized response teams trained in trauma-informed care and de-escalation techniques. Establishing dedicated crisis stabilization centers as alternatives to emergency rooms can provide veterans with rapid, focused support in a less stressful environment. Furthermore, fostering data-sharing collaborations among mental health providers, law enforcement, and veteran organizations is vital for early identification and intervention. The table below contrasts current practices with proposed improvements in crisis response:
| Existing Practice | Proposed Enhancement |
|---|---|
| Emergency rooms as primary crisis care | Specialized crisis stabilization units staffed by trained professionals |
| Limited tele-mental health services | Comprehensive telehealth platforms with veteran-specific resources |
| Generic mental health screening tools | Standardized, veteran-tailored assessment instruments |
| Fragmented data sharing among agencies | Integrated multi-agency dialog networks |
Conclusion: Prioritizing Mental Health Care for Veterans to Prevent Future Tragedies
The involvement of a Green Beret undergoing mental health treatment in the Las Vegas Cybertruck explosion has brought critical attention to the mental health needs of veterans. As investigations proceed, this case serves as a powerful reminder of the complex psychological challenges faced by those who have served in the military. It underscores the urgent necessity for accessible, effective, and continuous mental health services designed to support veterans through their transition to civilian life, ultimately aiming to reduce the risk of similar incidents in the future.